In honor of this month which is dedicated to sharing what dysphagia is and its impact on those affected, we would like to share a case study that highlights our corner of the dysphagia universe – mobile Fiberoptic Endoscopic Evaluation of Swallow (FEES) studies.
This patient was residing in a skilled nursing facility and began to complain of difficulty swallowing. A bedside swallow evaluation was completed, and the speech pathologist recommended that the patient move from a regular diet with thin liquids to a pureed diet with nectar thick liquids. Oral thrush was suspected, so the patient was prescribed oral Nystatin by their physician. The patient’s oral intake continued to decline with no clear reason; the facility speech pathologist requested a mobile FEES evaluation to help determine the presence and severity of the dysphagia and to assist with further care planning.
Here is a picture from the initial FEES:
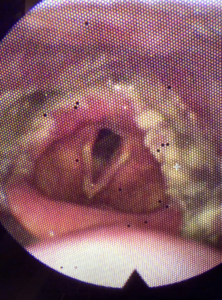
A fungal-like growth was coating the pyriform sinuses, posterior cricoid space, arytenoids, lateral channels, and aryepiglottic folds. Laryngeal mobility appeared restricted by this mounded coating. The patient was prescribed Diflucan, and a repeat FEES was requested 3 weeks later.
Here is what was found in the repeat FEES:
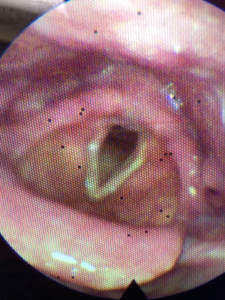
No more coating! And voilà, the patient’s swallow function had returned to normal – they were able to return to a regular diet with thin liquids without any difficulty.
This case study calls attention to several important pieces of the dysphagia management puzzle: the importance of imaging, the multi-professional approach that is typically required to help those with swallowing disorders, and the value of reassessment after interventions have been carried out. The facility speech pathologist recognized that the patient’s swallowing issues were not successfully managed at the bedside alone. This aligns with ASHA’s statement that “The non-instrumental assessment of swallowing is insufficient to infer specific information about laryngeal, pharyngeal, or upper esophageal anatomy and physiology required to develop effective treatment options and prevent consequences of dysphagia, such as dehydration, malnutrition, pneumonia, and death (Garand et al., 2020).”
Providing quality medical care takes a village, and dysphagia management is no exception.
After recognizing the need for dysphagia imaging and following the completion of the exam, we were able to work together with the facility to identify effective next steps for this patient. The follow-up FEES closed the loop for this particular case, as it provided the necessary visualization of the anatomy to confirm that the medication had worked and that swallow function had been restored.
We provide mobile dysphagia imaging in our communities so that we can bring our corner of the dysphagia universe directly to you and your patients. We are honored every time we are called in to assist you with your dysphagia management plan. Thank you for everything you do!
Lastly, in honor of this month – we are offering $20 off any of our self-study online courses! Use the promo code: cspdysphagia20 to redeem this promotion.

